Chapter I
NEW – BUT NO BETTER OR EVEN WORSE
Virtually every week there seems to be a news story highlighting an unanticipated drug side-effect, a surgical mishap, a rampant infection, or a mismanaged pregnancy. Some critics go further: they portray today’s science-based medicine as dehumanising – as if the butchery that preceded modern surgery or the poisons that once passed for therapeutic drugs were somehow more humane.
Yet modern medicine has been hugely successful. The development of effective drugs has revolutionised the treatment of heart attacks and high blood pressure and enabled many people with schizophrenia to emerge from mental hospitals to live at home. The effectiveness of drugs for stomach ulcers has done away with the need for major surgery, and futile treatments such as milk diets have been consigned to history. Childhood immunisation has made polio and diphtheria distant memories. It is easy to forget that leukaemia was once an almost uniformly fatal disease; and patients now regularly live with other cancers instead of dying from them. In west and equatorial Africa, the disease known as river blindness, which is caused by the larva of a type of fly, once left many people blind. It has now been virtually eradicated by drug treatment.
Modern imaging techniques have also brought significant benefits. Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) have helped to ensure that patients are accurately diagnosed and receive the right treatment. For example, MRI can reveal what type of stroke a patient has suffered. If the stroke is caused by bleeding into the brain (haemorrhagic stroke), then aspirin, which is useful in other types of stroke, might be dangerous. Surgical and anaesthetic techniques, too, have been greatly improved. Artificial joints have helped countless people, and organ transplants have become commonplace.
Of course many improvements in health have come about because of social and public health advances, such as piped clean water, sanitation, and better nutrition and housing. But even sceptics would be hard put to dismiss the impressive impact of modern medical care. Over the past half century, much of our increased life expectancy can be attributed to better healthcare, as can years of improved quality of life for those with chronic (persistent) diseases.
Even now, however, too much medical decision-making is based on poor evidence and there are still too many medical treatments that harm patients, and worthwhile treatments that are not used enough (see below, and Chapter 5). Almost invariably there will be uncertainties about effects and effectiveness when new treatments are devised – treatment effects are very seldom overwhelmingly obvious.
So, carefully designed fair tests are necessary to identify the effects reliably (see Chapter 3). Without a fair – unbiased – evaluation, the risk is that useless or even harmful treatments are deemed helpful or, conversely, that helpful treatments are dismissed as useless. Untested theories about treatments effects, however convincing they may sound, are not enough. Some theories have predicted that treatments would work, but actual evidence has revealed otherwise; other theories have confidently predicted that treatments would not work when, in fact, tests showed that they did.
There is nothing new in this: in the 18th century James Lind used a fair test to compare six of the remedies then being used to treat scurvy, a disease that was killing vast numbers of sailors during long voyages. He showed that (vitamin-C-containing) oranges and lemons were a very effective cure. In essence, Lind conducted what is now called a controlled trial.
In 1747, while serving as a ship’s surgeon aboard HM 4th Rate Ship Salisbury, James Lind assembled 12 of his patients at similar stages of the illness, accommodated them in the same part of the ship, and ensured that they had the same basic diet. This was crucial – it creating a ‘level playing field’ (see Chapter 3, and Chapter 4, box on page 59). Lind then allocated two sailors to receive each of six treatments that were then in use for scurvy – cider, sulphuric acid, vinegar, seawater, nutmeg, or two oranges and a lemon. The fruit won hands down, and the Admiralty later ordered that lemon juice be supplied to all ships, with the result that the deadly disease had disappeared from the Royal Navy by the end of the 18th century. Of the treatments Lind compared, the Royal College of Physicians favoured sulphuric acid while the Admiralty favoured vinegar – Lind’s fair test showed that both these authorities were wrong. And medical authority is not infrequently wrong (see below, and Chapters 2, 5, and 6).
Similar uncertainties about the effects of treatments are often highlighted today when doctors and other clinicians differ about the best approach for a particular condition (see Chapter 4). In addressing these uncertainties the public as well as doctors have an important part to play. It is in the overwhelming interest of patients as well as professionals that research on treatments should be rigorous. Just as doctors must be assured that their treatment recommendations are based on sound evidence, so patients need to demand that this happens. Only by creating this critical partnership can the public have confidence in all that modern medicine has to offer (see Chapter 7).
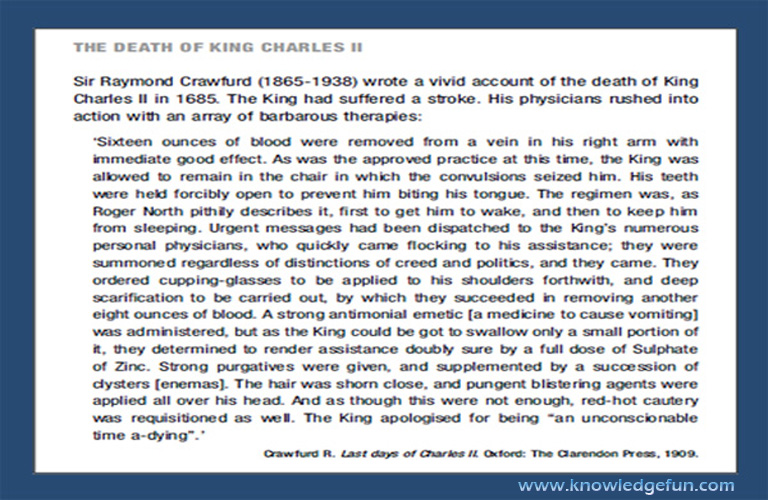
The Death of King Charles II
Sir Raymond Crawfurd (1865-1938) wrote a vivid account of the death of King Charles II in 1685. The King had suffered a stroke. His physicians rushed into action with an array of barbarous therapies:
'Sixteen ounces of blood were removed from a vein in his right arm with immediate good effect. As was the approved practice at this time, the King was allowed to remain in the chair in which the convulsions seized him. His teeth were held forcibly open to prevent him biting his tongue. The regimen was, as Roger North pithily describes it, first to get him to wake, and then to keep him from sleeping. Urgent messages had been dispatched to the King’s numerous personal physicians, who quickly came flocking to his assistance; they were summoned regardless of distinctions of creed and politics, and they came. They ordered cupping-glasses to be applied to his shoulders forthwith, and deep scarification to be carried out, by which they succeeded in removing another eight ounces of blood. A strong antimonial emetic [a medicine to cause vomiting] was administered, but as the King could be got to swallow only a small portion of it, they determined to render assistance doubly sure by a full dose of Sulphate of Zinc. Strong purgatives were given, and supplemented by a succession of clysters [enemas]. The hair was shorn close, and pungent blistering agents were applied all over his head. And as though this were not enough, red-hot cautery was requisitioned as well. The King apologised for being ‘‘an unconscionable time a-dying’’.'
Crawfurd R. Last days of Charles II. Oxford: The Clarendon Press, 1909.